Contents
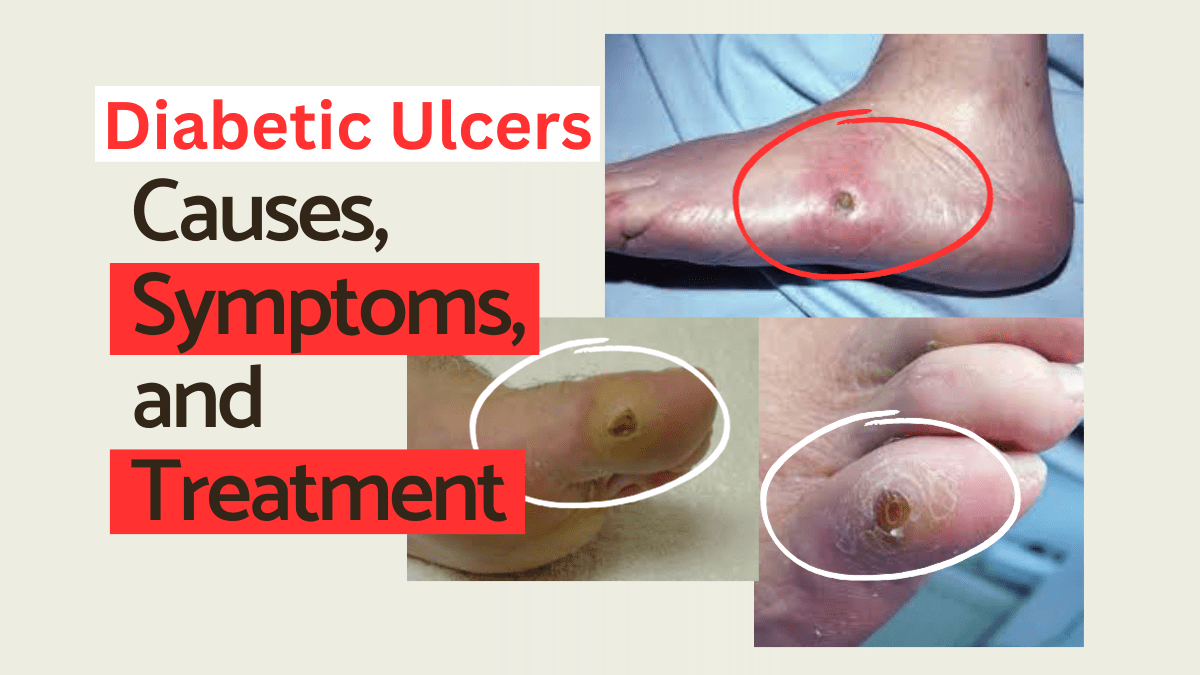
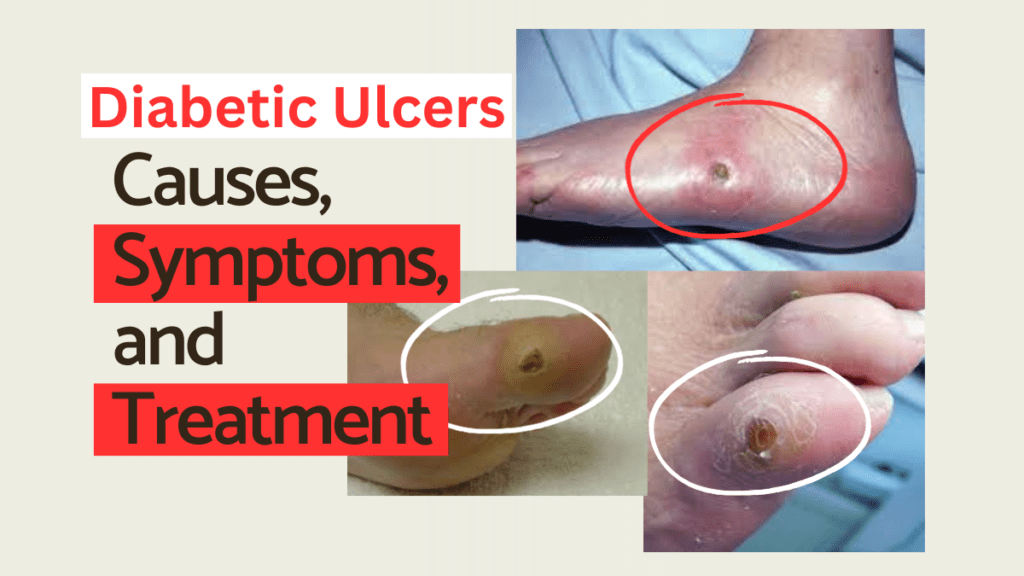
Diabetic Ulcers
“Diabetic ulcers can be serious and debilitating, but with proper care and treatment, they can be managed effectively. In this article, we will explore what diabetic ulcers are, their causes and symptoms, and the available treatment options. Whether you have been diagnosed with diabetes or simply want to learn more, read on to gain valuable insights into this common yet often misunderstood condition.”
What is a Diabetic Ulcer?
A diabetic ulcer is a type of open wound that occurs on the skin of individuals living with diabetes. It is primarily associated with a condition called diabetic neuropathy, which refers to nerve damage that is commonly seen in diabetes. Diabetic neuropathy can cause a loss of sensation and impaired blood circulation, leading to the formation of ulcers that are slow to heal and prone to infection.
Causes of Diabetic Ulcers
Diabetic ulcers typically develop due to a combination of factors, including:
- Peripheral neuropathy: Nerve damage that impairs sensation in the feet, making it difficult to detect injuries or wounds.
- Peripheral artery disease: Reduced blood flow to the lower extremities, which slows down the healing process.
- Foot deformities: Conditions such as bunions or hammertoes that cause pressure points and increase the risk of developing ulcers. Also Known as foot diabetic Ulcer.
- Inadequate foot care: Neglecting proper foot hygiene and not taking necessary precautions can contribute to the development of ulcers.
Symptoms of Diabetic Ulcers
Diabetic ulcers usually appear on the feet and lower legs, but they can occur elsewhere on the body. Recognizing the early signs of a diabetic ulcer is crucial for prompt treatment. Look out for the following symptoms:
- Pain or tenderness: Ulcers may be painful, especially when pressure is applied.
- Redness or inflammation: The surrounding skin may become red, swollen, or warm to the touch.
- Drainage: Pus or fluid may be present, indicating an infection.
- Foul odor: A strong smell from the ulcer site can be an indication of infection.
- Delayed healing: Slow wound healing despite proper care and treatment.
If you experience any of these symptoms, it is important to seek medical attention promptly.

Treatment Options for Diabetic Ulcers
The proper management of diabetic ulcers requires a multi-faceted approach involving medical interventions, wound care, and lifestyle modifications. Here are some common treatment options:
1. Wound Debridement
“Wound debridement involves the removal of damaged or dead tissue from the ulcer site, which promotes healing and prevents infection. This can be done through a variety of methods, including surgical debridement, enzymatic debridement, or autolytic debridement.”
2. Infection Control
“Infections are common complications of diabetic ulcers and can significantly impede the healing process. Treating or preventing infections is essential. In some cases, your healthcare provider may prescribe antibiotics to combat the infection.”
3. Offloading
“Offloading is a technique used to relieve pressure on the affected area, allowing the ulcer to heal. This can be achieved with the use of specialized footwear, orthotic devices, or casts to redistribute the weight-bearing load.”
4. Dressings and Topical Treatments
“Using appropriate dressings and topical treatments can help create a favorable environment for wound healing. These can include antimicrobial dressings, moist dressings, or growth factor applications.”
Yellow Fever Mosquito FAQ’s : Why is yellow fever dangerous ? 5
5. Blood Sugar Control
“Maintaining optimal blood sugar levels is crucial for proper wound healing and preventing further complications. Your healthcare provider may adjust your diabetes management plan to achieve better glycemic control.”
6. Compression Therapy
“For individuals with venous ulcers, compression therapy can aid in improving blood flow and reducing swelling. Compression stockings or bandages are commonly used for this purpose.”
7. Advanced Therapies
In certain cases, advanced therapies may be required for non-healing ulcers. These may include:
- Hyperbaric oxygen therapy: Involves breathing pure oxygen in a pressurized chamber, increasing oxygen levels in the blood and promoting wound healing.
- Skin grafts or substitutes: Surgical procedures that involve the transplantation of healthy skin or the application of bioengineered skin substitutes.
- Negative pressure wound therapy: Involves the use of a vacuum dressing to promote wound healing by removing excess fluid and enhancing blood flow.
Note: Treatment options may vary depending on the individual and the severity of the ulcer. It is important to consult with a healthcare professional for personalized advice.
Conclusion
“Diabetic ulcers can have a significant impact on individuals living with diabetes, but understanding the causes, symptoms, and available treatment options can help manage and even prevent them. It is essential to prioritize foot care, regularly monitor for any signs of ulcers, and seek medical attention promptly to prevent complications. By taking proactive steps to protect and care for your feet, you can minimize the risk of diabetic ulcers and maintain a healthy, active lifestyle.”
Follow Us On X