Contents
- 1 The Anti-Cancer Toolkit: 5 Must-Know Ways to Prevent a Diagnosis
- 2 1. Eliminate Tobacco and Limit Alcohol: The Immediate Impact
- 3 2. Embrace a Plant-Powered, Weight-Controlling Diet
- 4 3. Regular Physical Activity: A Natural Defense
- 5 4. Protect Against Infections and Environmental Exposure
- 6 5. Routine Cancer Screenings: Early Detection is Curative
- 7 The Power of Prevention: Statistical Insight
- 8 ❓ Frequently Asked Questions (FAQ)
- 8.1 Q1: Is the risk of cancer completely eliminated if I follow the Anti-Cancer Toolkit perfectly?
- 8.2 Q2: I smoked for 20 years, is it too late for me to start using this Anti-Cancer Toolkit?
- 8.3 Q3: How do I know if I have a “healthy weight” beyond just using BMI?
- 8.4 Q4: Are expensive organic foods necessary for an effective Anti-Cancer Diet?
- 8.5 Q5: If cancer runs in my family, does screening even help?
- 9 Conclusion: Activating Your Anti-Cancer Toolkit
The Anti-Cancer Toolkit: 5 Must-Know Ways to Prevent a Diagnosis
The shadow of a cancer diagnosis looms large, yet a significant portion of cancer cases—estimated to be between 30% and 50%—are considered preventable through lifestyle choices and screening (Source: World Health Organization (WHO)). This staggering figure empowers us. It means we hold an invaluable Anti-Cancer Toolkit that can dramatically reduce our individual risk.
This comprehensive guide is your blueprint for proactive health. We will delve into five fundamental, research-backed strategies that form the core of a robust cancer prevention plan. By adopting these measures, you don’t just reduce your cancer risk; you invest in a longer, healthier, and more vital life. Mastering this Anti-Cancer Toolkit is about making informed, consistent choices that tip the scales in your favor. Understanding and applying the principles of this Anti-Cancer Toolkit is key to longevity.
1. Eliminate Tobacco and Limit Alcohol: The Immediate Impact
The most potent weapon in your Anti-Cancer Toolkit is the immediate and complete cessation of tobacco use in all its forms. The link between smoking and cancer is undeniable, but alcohol also plays a significant, often underestimated, role.
Quitting Tobacco: The Single Biggest Win
Tobacco smoke contains over 7,000 chemicals, with at least 69 known to cause cancer (Source: WHO). Tobacco use is the single greatest avoidable risk factor for cancer mortality globally. It’s not just lung cancer; tobacco is causally linked to cancers of the mouth, throat, esophagus, pancreas, bladder, cervix, kidney, and more. Even secondhand smoke exposes non-smokers to carcinogenic compounds, making a smoke-free environment a crucial part of the communal Anti-Cancer Toolkit.
- Actionable Step: If you smoke, seek professional help and FDA-approved cessation aids immediately. The benefits of quitting begin almost instantly and continue for decades. Your body begins repairing damage right away, proving the power of this step in the Anti-Cancer Toolkit.
Understanding Alcohol’s Carcinogenic Nature
Alcohol is classified as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC), meaning it is definitively cancer-causing. It is causally linked to at least seven types of cancer, including breast, liver, colorectal, esophageal, and head and neck cancers (Source: WHO). Alcohol’s risk factor is dose-dependent: the more you drink, the higher the risk. For some cancers, even light to moderate consumption can increase risk. The mechanism often involves acetaldehyde, a toxic breakdown product of alcohol, and increased estrogen levels. Implementing limits on alcohol is a necessary boundary in your personal Anti-Cancer Toolkit.
- Actionable Step: To minimize risk, it is best to avoid alcohol completely. If you choose to drink, limit consumption to no more than one standard drink per day for women and two standard drinks per day for men (one standard drink equals 12 oz beer, 5 oz wine, or 1.5 oz of 80-proof spirits).
Graph: Alcohol Consumption and Increased Relative Cancer Risk
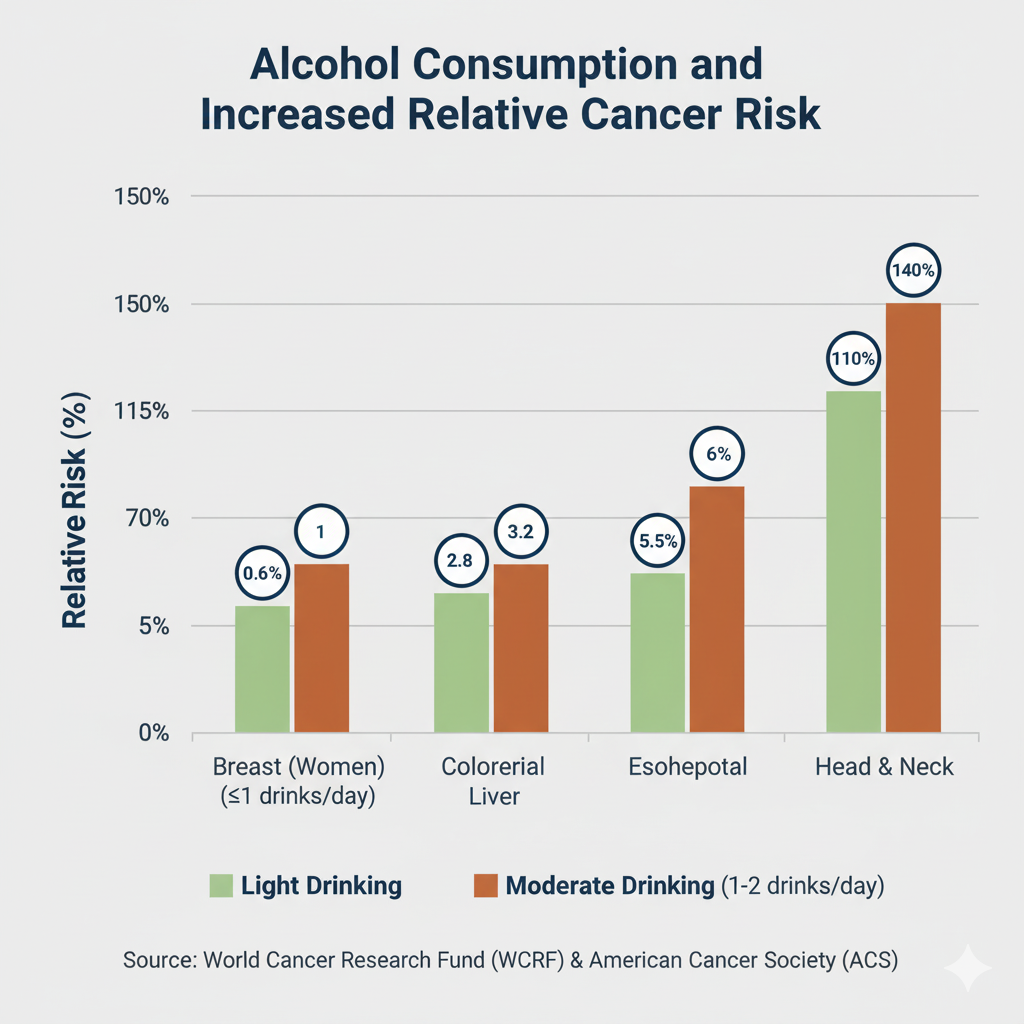
Caption: This graph illustrates how the risk for several major cancers escalates even with light to moderate alcohol consumption, emphasizing the need to limit or eliminate intake as part of the Anti-Cancer Toolkit.
2. Embrace a Plant-Powered, Weight-Controlling Diet
Dietary choices and weight management are inextricably linked, forming a crucial pillar of your Anti-Cancer Toolkit. Excessive body fat is a major, yet modifiable, risk factor linked to at least 13 different types of cancer, including breast, colon, endometrial, and kidney cancers (Source: American Cancer Society (ACS)). The chronic, low-grade inflammation driven by excess fat tissue is a key mechanism for cancer promotion.
The Cornerstones of an Anti-Cancer Diet
A healthy eating pattern for cancer prevention is less about restrictive dieting and more about abundance—filling your plate with nutrient-dense, plant-based foods.
| Food Category | Recommended Intake & Focus | Anti-Cancer Benefits |
| Vegetables & Fruits | Aim for at least 2½ to 3 cups of vegetables and 1½ to 2 cups of fruit daily. Focus on a variety of colors and cruciferous vegetables (broccoli, kale). | Rich in antioxidants, vitamins, and fiber. Antioxidants neutralize cell-damaging free radicals, while fiber aids gut health and carcinogen elimination. |
| Whole Grains | Make whole grains (brown rice, oats, quinoa, whole wheat) at least half of your grain intake. | High in fiber and various nutrients. Whole grains are strongly linked to a reduced risk of colorectal cancer. |
| Protein Sources | Choose fish, poultry, beans, and legumes over red and processed meats. | Provides essential protein without the high saturated fat and potential carcinogens found in processed meats. |
| Fats | Prioritize healthy fats like those found in olive oil, nuts, and avocados (mono- and polyunsaturated fats). | Support overall health and help with the absorption of fat-soluble vitamins, fueling the Anti-Cancer Toolkit internally. |
Limiting Carcinogenic Foods:
- Processed Meats: Bacon, sausage, hot dogs, and deli meats are classified as Group 1 carcinogens (cancer-causing to humans) due to chemical preservatives (nitrates/nitrites) and cooking processes. Limit consumption drastically, if not eliminate it entirely.
- Red Meat: Limit fresh red meat (beef, pork, lamb) intake to no more than 18 ounces (cooked) per week. Red meat is classified as “probably carcinogenic to humans” (Group 2A) (Source: IARC, as cited by ACS).
Maintaining a Healthy Weight
The most important part of diet for cancer prevention is managing your caloric intake to maintain a healthy weight (Source: NIH). Adipose tissue (body fat) produces excess hormones like estrogen, which can fuel certain cancers, and contributes to chronic inflammation, a known cancer precursor. This management is a critical step in maintaining your Anti-Cancer Toolkit effectively.
- Calculation: Monitor your Body Mass Index (BMI). While BMI is a general measure, maintaining it within the healthy range (18.5 to 24.9) significantly reduces your risk for numerous obesity-related cancers. Tracking your waist circumference is also vital, as abdominal fat poses a higher risk.
3. Regular Physical Activity: A Natural Defense
Physical activity is a non-negotiable component of a truly effective Anti-Cancer Toolkit. Beyond its benefits for weight control, regular exercise directly impacts several biological mechanisms that help prevent cancer.
Exercise: More Than Just Calorie Burning
Regular physical activity helps in the following ways:
- Hormone Regulation: Helps maintain healthy levels of hormones (like estrogen and insulin), preventing the hormonal imbalances that can drive cancer growth.
- Immune Function: Boosts immune function, allowing the body to better identify and destroy abnormal cells before they become tumors. A strong immune system is the front line of the Anti-Cancer Toolkit.
- Bowel Transit Time: For colorectal cancer prevention, exercise helps food move through the digestive system faster, reducing the contact time between the colon lining and potential carcinogens.
Minimum Activity Guidelines
The American Institute for Cancer Research (AICR) recommends a clear set of guidelines:
| Intensity Level | Recommended Weekly Minutes | Example Activities |
| Moderate Intensity | 150 minutes per week (e.g., 30 minutes, 5 days a week) | Brisk walking, water aerobics, gardening, dancing. |
| Vigorous Intensity | 75 minutes per week | Running, hiking uphill, swimming laps, intense circuit training. |
- Beyond Exercise: Move More, Sit Less: Emerging evidence suggests that prolonged sedentary behavior—even for people who meet the recommended exercise guidelines—may increase the risk of certain cancers. Incorporate movement into your daily routine by standing up, stretching, or walking for a few minutes every hour. This simple habit reinforces the active lifestyle required by the Anti-Cancer Toolkit.
4. Protect Against Infections and Environmental Exposure
While lifestyle choices dominate the conversation, protecting yourself from specific biological and physical carcinogens is also a key strategy in the Anti-Cancer Toolkit.
Vaccinations: Cancer Prevention by Injection
Certain infections are classified as biological carcinogens because they cause chronic inflammation or directly alter cellular DNA, leading to cancer. Vaccination is a powerful tool to prevent these cancers.
- HPV Vaccine: Human Papillomavirus (HPV) is the primary cause of cervical cancer and is also linked to cancers of the throat, anus, vagina, vulva, and penis. The HPV vaccine can prevent over 90% of HPV-related cancers when given at recommended ages (Source: ACS).
- Hepatitis B Vaccine: Chronic infection with Hepatitis B virus (HBV) is a leading cause of liver cancer. The HBV vaccine is a vital preventive measure against infection-related cancers, making it a medical essential in the Anti-Cancer Toolkit.
Sun Safety and Environmental Toxins
- UV Radiation: Ultraviolet (UV) radiation from the sun and tanning beds is the main cause of skin cancer, including serious melanoma. This damage is cumulative over time. Use broad-spectrum sunscreen, wear protective clothing, and seek shade, especially between 10 a.m. and 4 p.m.
- Air Pollution & Workplace Exposure: Outdoor and indoor air pollution (e.g., from cooking with solid fuels) contribute to lung cancer deaths (Source: WHO). Occupational carcinogens like asbestos and benzene are linked to mesothelioma and leukemia, respectively. Be aware of your exposure risks at home and work and take necessary precautions (e.g., proper ventilation, personal protective equipment). Being aware of these external threats strengthens your defensive Anti-Cancer Toolkit.
5. Routine Cancer Screenings: Early Detection is Curative
The final, essential component of your Anti-Cancer Toolkit is regular screening. Screening tests find cancer or pre-cancerous conditions in people who have no symptoms, offering the best chance for successful treatment. Early detection is often the difference between a high survival rate and a grim prognosis.
Your Personalized Screening Schedule
Screening guidelines are based on age, sex assigned at birth, and individual risk factors. Always discuss your specific history and optimal schedule with your healthcare provider. This proactive consultation is a crucial part of leveraging your Anti-Cancer Toolkit.
| Cancer Type | Target Group (Average Risk) | Recommended Screening Schedule | Backlinks |
| Colorectal Cancer | All individuals | Start at age 45. Options include colonoscopy every 10 years, or stool-based tests (FIT/FOBT) yearly. | ACS Screening Guidelines |
| Breast Cancer | Women/Individuals assigned female at birth | Annual mammograms starting at age 45 (choice to start at 40). Biennial screening from age 55. | ACS Screening Guidelines |
| Cervical Cancer | Individuals with a cervix | Start at age 25. Primary HPV test every 5 years, or Co-test (Pap + HPV) every 5 years. | ACS Screening Guidelines |
| Lung Cancer | Current or former heavy smokers | Yearly Low-Dose CT (LDCT) scan for individuals age 50-80 with a 20-pack-year smoking history who currently smoke or have quit within the last 15 years. | ACS Screening Guidelines |
| Prostate Cancer | Men/Individuals with a prostate gland | Discussion with a healthcare provider about the pros and cons of PSA testing should begin at age 50 (earlier for high-risk groups). | ACS Screening Guidelines |
*Note: This table provides general guidelines for average-risk individuals. High-risk individuals (due to family history or genetic predisposition) may need to start screening earlier or undergo more frequent testing.
Infographic: The Anti-Cancer Toolkit Flowchart
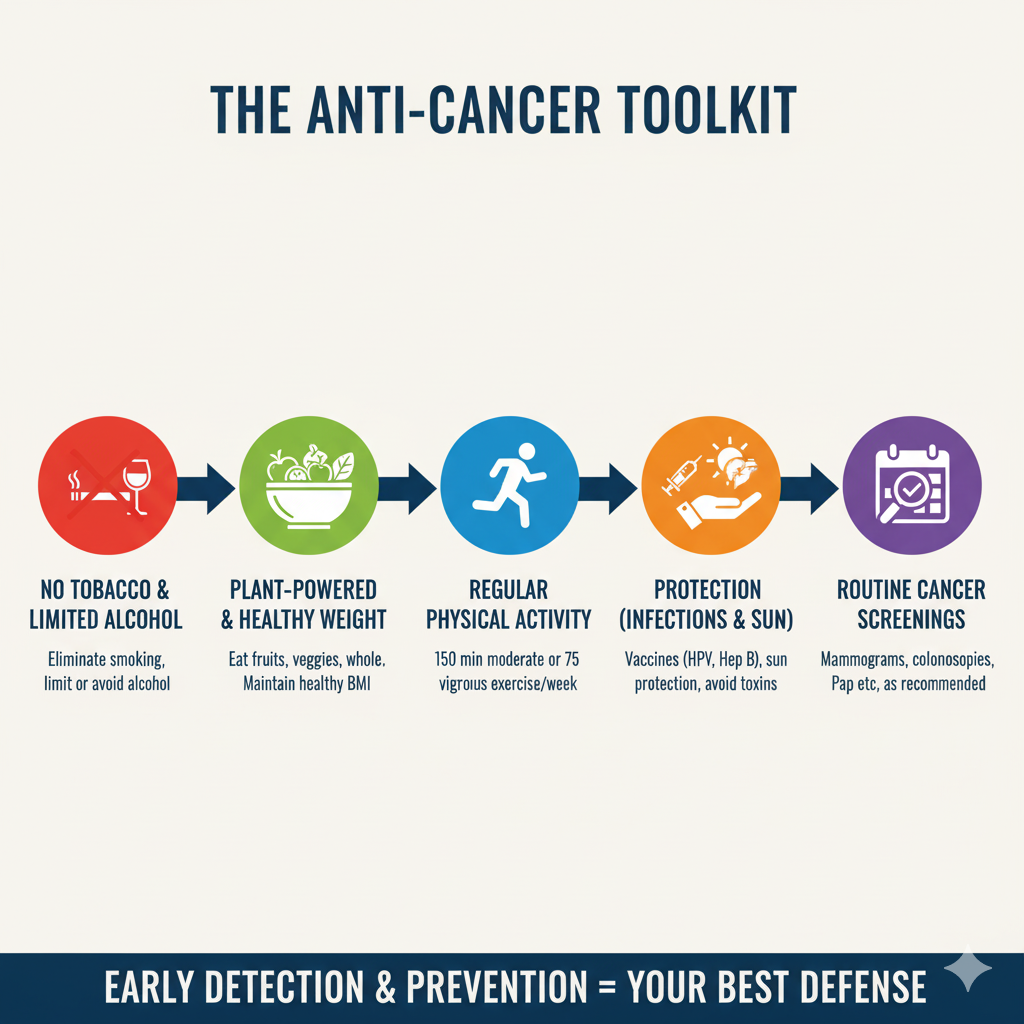
Caption: The Anti-Cancer Toolkit summarized: A five-step approach that combines proactive lifestyle choices with crucial early detection methods for maximum protection.
The Power of Prevention: Statistical Insight
It’s often easier to commit to change when the impact is quantified. Statistical analysis clearly demonstrates the protective power of lifestyle in preventing cancer. Studies show that between $\mathbf{40\%}$ and $\mathbf{50\%}$ of cancers are linked to modifiable risk factors and are thus preventable (Source: American Cancer Society).
The following table, powered by data from major research bodies, highlights the significant proportion of cancer cases that are attributable to the modifiable risk factors addressed in this Anti-Cancer Toolkit.
Table: Estimated Proportion of U.S. Cancer Cases Attributable to Modifiable Risk Factors (2019 Estimates)
| Modifiable Risk Factor | Estimated Percentage of All Cancer Cases Attributable | Cancers Most Highly Affected (Attributable %) |
| Cigarette Smoking | 19.3% | Lung (88.2%), Larynx (89.9%), Esophagus (85.4%), Bladder (46.9%) |
| Excess Body Weight (High BMI) | 7.6% | Uterine (60.3%), Liver (33.9%), Kidney (32.3%), Postmenopausal Breast (11.3%) |
| Alcohol Consumption | 5.4% | Oral Cavity/Pharynx (46.3% in men), Esophagus, Liver, Breast |
| UV Radiation (Sun/Tanning Beds) | 4.6% | Skin Melanoma (92.2%), Non-Melanoma Skin Cancers |
| Physical Inactivity | 3.1% | Uterine (26.7%), Colorectal (16.3%), Breast (3.9%) |
| Unhealthy Diet (Low Fiber, High Red/Processed Meat) | $\sim$5% (Dietary Risks Combined) | Colorectal (up to 18.5%), Stomach, Pharynx |
| Infection (e.g., HPV, HBV) | Varies Widely | Cervical (100%), Anal (88.2%), Liver (Hepatitis B/C) |
Data compiled from American Cancer Society (ACS) and Global Burden of Disease (GBD) studies, focusing on adults aged 30 and older.
This data powerfully reinforces the core message of the Anti-Cancer Toolkit: small, intentional changes across these five areas have the potential to prevent hundreds of thousands of cancer cases annually.
❓ Frequently Asked Questions (FAQ)
Q1: Is the risk of cancer completely eliminated if I follow the Anti-Cancer Toolkit perfectly?
A: No, unfortunately, not all cancer is preventable. While the Anti-Cancer Toolkit significantly reduces your risk—up to 50% of cancers are linked to lifestyle—the remaining portion is related to non-modifiable factors like aging, genetics, and random cellular mutations. Following this guide is about stacking the odds in your favor, maximizing the impact of your modifiable factors, and ensuring early detection for the best outcomes.
Q2: I smoked for 20 years, is it too late for me to start using this Anti-Cancer Toolkit?
A: It is never too late. The benefits of quitting smoking begin within 20 minutes of your last cigarette, and your risk of cancer decreases significantly over time. For example, your risk of lung cancer drops by half within 10 to 15 years of quitting, and the risk of mouth, throat, and esophageal cancer drops by half within five years. This demonstrates the immediate and lasting power of adding that first step to your Anti-Cancer Toolkit.
Q3: How do I know if I have a “healthy weight” beyond just using BMI?
A: While Body Mass Index (BMI) is a useful screening tool (healthy range 18.5–24.9), a more specific measure for cancer risk is waist circumference. Excess fat stored around the abdomen (visceral fat) is hormonally and metabolically more active and poses a higher cancer risk. The general rule of thumb is that a waist circumference greater than 35 inches for women or 40 inches for men indicates an elevated risk, regardless of BMI. This metric is a practical part of the Anti-Cancer Toolkit.
Q4: Are expensive organic foods necessary for an effective Anti-Cancer Diet?
A: No. The primary focus of the anti-cancer diet is the quantity and variety of plant-based foods, not whether they are organic. Consuming a wide range of affordable, conventional fruits, vegetables, and whole grains provides immense protective benefits through fiber and phytochemicals. The advice is to eat a lot of plants; if you can afford organic, that’s a bonus, but it should not be a barrier to following this crucial part of the Anti-Cancer Toolkit.
Q5: If cancer runs in my family, does screening even help?
A: Yes, absolutely. If cancer runs in your family, screening is even more critical. A family history often places you in a “high-risk” category, meaning your recommended screening schedule may be earlier or more frequent than the general population. For example, colonoscopy screening might start at age 40 instead of 45. Your physician can use this information to tailor your personal Anti-Cancer Toolkit and ensure detection at the earliest, most treatable stage.
Conclusion: Activating Your Anti-Cancer Toolkit
The statistics can be intimidating, but they also highlight an incredible truth: prevention works. By focusing on the core elements of the Anti-Cancer Toolkit—eliminating tobacco and limiting alcohol, embracing a plant-rich diet, committing to regular physical activity, guarding against infections and environmental exposures, and adhering to recommended screening schedules—you are taking decisive, evidence-based control of your health destiny.
This is not about making massive, unsustainable changes overnight, but rather adopting small, consistent habits that compound over time. Every healthy choice you make is a victory, a reinforcement of your personal Anti-Cancer Toolkit. Empower yourself with knowledge and action, and step confidently into a future with reduced cancer risk.
Take the Next Step in Prevention: Download our FREE Anti-Cancer Toolkit Checklist to track your progress on diet, exercise, and screening. Don’t wait—proactive health starts now.
Trichomoniasis: Symptoms, Causes, Treatment, and Prevention